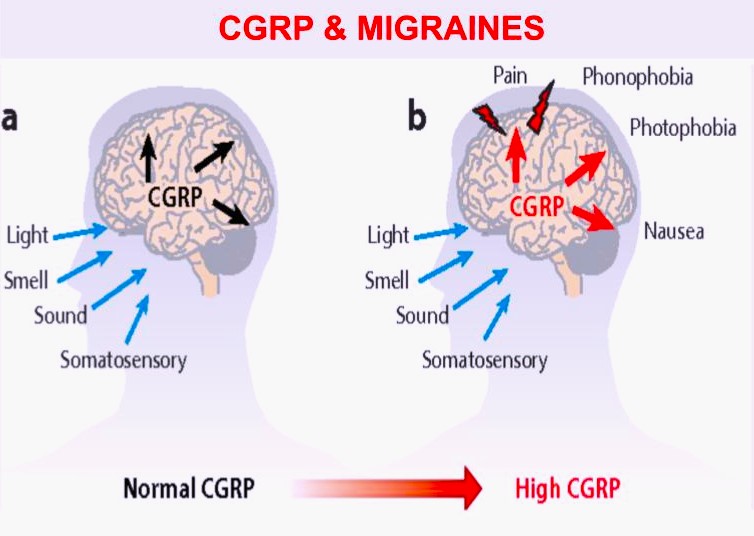
Many patients feel that certain foods trigger their migraines. In fact, migraineurs often avoid particular foods or ingredients to avoid headaches.
Common food triggers include alcohol, caffeine and compounds found in foods including nitrates (found in cured meats), histamine (in dried fruits, fermented foods), tyramine (in wine), phenylethylamine (in lentils, beans, nuts).
There is mixed evidence regarding food triggers.
In a 2020 meta analysis in the Journal of Head and Face Pain, forty-three studies looking at dietary migraine triggers were examined, and alcohol and caffeine were found to be most common diet related triggers. However, it was concluded that currently there is poor evidence from studies and more high-quality research is needed. A 2020 study of chocolate as migraine trigger found that although a small number of patients reported chocolate as migraine trigger, but provocative studies could not confirm chocolate as migraine trigger, in fact, eating chocolate may be more associated with food craving or premonitory symptoms.
The best way to determine if food triggers are affecting you is by keeping a headache diary. Because we are all unique, some common food triggers that may affect one person, may not affect another.
To learn more about migraines and food triggers, speak with your healthcare provider.
By: Brooke Steiger, FNP