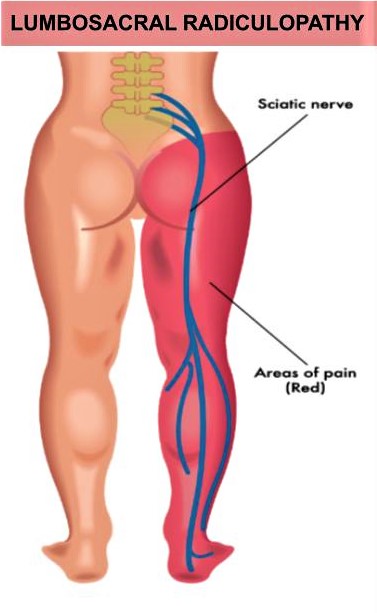
Lumbosacral radiculopathy is one of the most common problems seen in a neurologic consultation.
Acute lumbosacral radiculopathy can be separated into three general categories from least to most severe. The first being sensory/painful radicular pattern, characterized by radicular pain and a segmental pattern of sensory dysfunction but no other neurologic deficits. In addition, patients may experience mild motor deficit patterns, characterized by radicular pain, sensory dysfunction, and mild nonprogressive segmental motor weakness and/or reflex change. Lastly patients may have marked motor deficit patterns, characterized by radicular pain and sensory dysfunction with severe or worsening motor deficits.
Lumbosacral radiculopathy is a condition in which a disease process causes functional impairment of one or more lumbosacral nerve roots. The most common cause is structural (ie, disc herniation or degenerative spinal stenosis) leading to root compression. The acute time period starts at the time of symptom onset and extends up to four or six weeks.
The diagnosis of a lumbosacral radiculopathy is clinical, and can usually be made based upon compatible symptoms and examination findings. However, patients should be evaluated for less common mechanisms associated with permanent and progressive neurologic disability, as prompt diagnosis and treatment may improve outcome.
In patients who do not have an indication for urgent treatment, conservative symptomatic treatment is used during the acute period. While acute lumbosacral radiculopathy is often extremely painful, symptoms spontaneously improve in many cases. As examples, the clinical course may variably wax and wane when due to lumbar spinal stenosis from degenerative arthritis and may be self-limited when due to disc herniation.
To learn more, call The Manhattan Center for Headache and Neurology to schedule an evaluation with one or our exceptional providers!
By: Jordan Shankle, PA